
Bridging Frameworks: A Comparative Reflection on the Determinants of Health in Ontario and British Columbia
For this interprofessional activity, I collaborated with a Nuclear Medicine Technologist (NMT) from British Columbia to compare how Ontario and British Columbia define, prioritize, and operationalize the social determinants of health (SDoH), and the activity showed clear regional differences in approach, as well as how each province operationalizes equity as a principle into daily policy and action. As a Medical Laboratory Technologist in Ontario, I gained an increased understanding of how systemic choices shape equitable care across Canada. Both provinces follow the Public Health Agency of Canada’s (2023) SDoH framework, which states that health is shaped by social, economic, and environmental conditions, however, they differ in how these determinants are embedded into their health systems.
British Columbia: Structural Integration and Systemic Mandates
British Columbia has implemented a system-wide health equity strategy with a focus on accountability, integrating mandatory cultural safety across the health system. The B.C. Social Determinants of Health Value Set standardizes data elements, such as housing status, education, Indigenous identity, and others, so that equity indicators are consistently captured across health records and can meaningfully inform both clinical care and population health planning, as outlined by the Government of British Columbia in 2024. This structural foundation is supported by the Cultural Safety & Humility Standard and mandatory Indigenous cultural safety training, emphasizing BC’s commitment to integrating equity into the day-to-day fabric of practice, according to the Government of British Columbia in 2022 and Gore & Kothari in 2012. Consequently, these levers operationalize reconciliation and create clear accountability for organizations to deliver care that upholds anti-racism and equity principles.
Ontario: Actionable Tools and Frontline Implementation
In contrast, Ontario has developed practical, ground-level frameworks to enable organizations to address inequities in real time, and the Ontario Health Social Determinants of Health Framework & Resource Guide (2025) lays out a clear pathway for the identification, documentation, and addressing of social needs within the healthcare system. The Health Equity Impact Assessment (HEIA) and the Indigenous Lens Tool similarly provide a means to anticipate and mitigate potential inequities when planning or evaluating programs, as outlined by the Ministry of Health and Long-Term Care (2012) and Jumah et al. (2023)
These tools are grounded in the Ontario Public Health Standards (2021) and Health Equity Guideline (2018) which establish health equity as a cross-cutting requirement for all public health programs. Ontario’s emphasis is on turning policy into action at the front lines of practice and assisting organizations to embed equity into the routine of day-to-day practice, including the use of structured planning, equity-focused assessments and transparent reporting to identify and address inequities, target interventions to priority populations and monitor change over time, and together, these frameworks help to normalize equity-informed decision-making, build accountability and sustain measurable improvements in population health.
Shared Goals, Different Pathways
British Columbia’s approach emphasizes the significance of structural embedding and clear, standardized expectations, whereas Ontario’s approach prioritizes practical implementation and data-driven action. Each approach reflects the shared national imperative to reduce inequities, consistent with the study by Alemu et al. (2024) that the SDoH are integral to addressing unmet health needs.
To illustrate these differences more clearly, the following table summarizes how Ontario and British Columbia translate health equity principles into practice through different mechanisms of policy and implementation.
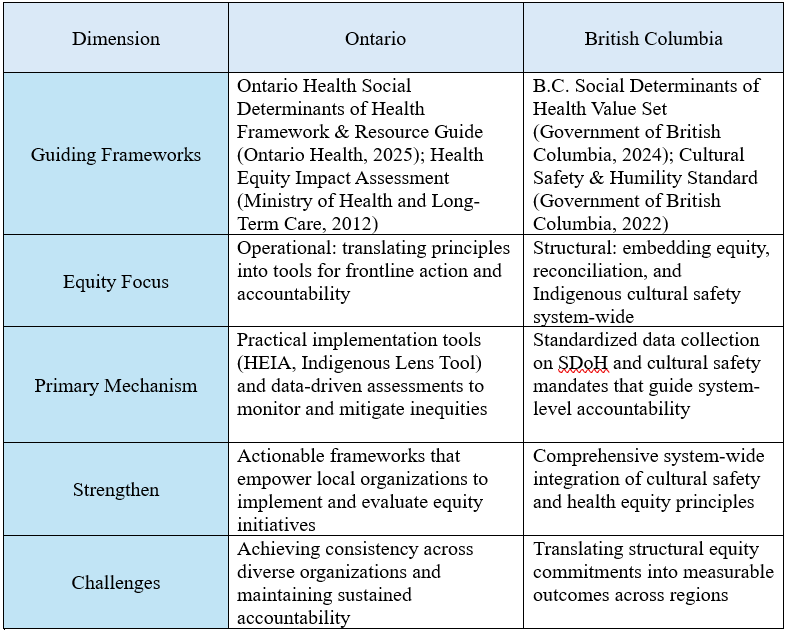
Note. Information synthesized from Ontario Health (2025), Ministry of Health and Long-Term Care (2012), Government of British Columbia (2022, 2024).sn
This comparative view shows that although Ontario and BC pursue the same equity objectives, their methods reveal complementary strengths. Ontario’s focus on actionable tools drives measurable progress at the local level, while BC’s structural accountability ensures that equity is embedded in governance and standards. Together, they demonstrate that achieving equity requires both the system-wide vision and the operational tools to make it real.
This collaboration demonstrated that to achieve equitable outcomes, more than identifying determinants is required; it demands institutionalizing compassion through strong data systems, ongoing training, and transparent accountability, because it is through these mechanisms that shared goals become actionable practices. As an Ontario MLT working with a BC NMT, I learned that provincial context and professional roles each play a part in the pursuit of equity in different but complementary ways, which makes shared goals actionable practices that bridge gaps and improve patient experience.
References:
Alemu, F. W., et al. (2024). Social determinants of unmet need for primary care: A systematic review. Systematic Reviews, 13, 252. https://doi.org/10.1186/s13643-024-02647-5
Gore, D., & Kothari, A. (2012). Social determinants of health in Canada: Are healthy living initiatives there yet? International Journal for Equity in Health, 11(1), 41. https://doi.org/10.1186/1475-9276-11-41
Government of British Columbia. (2022). Cultural Safety & Humility Standard (HSO 75000:2022). Province of British Columbia. https://www2.gov.bc.ca/gov/content/governments/technology-innovation/standards/cultural-safety
Government of British Columbia. (2024, September 4). B.C. Social Determinants of Health Value Set. Province of British Columbia. https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/health-information-standards/standards-catalogue/bc-social-determinants-of-health-standards
Government of Canada. (2023). Social determinants of health and health inequalities. Public Health Agency of Canada. https://www.canada.ca/en/public-health/services/health-promotion/population-health/what-determines-health.html
Government of Ontario. (2021). Ontario public health standards 2021. Ontario Ministry of Health. https://www.health.gov.on.ca/en/pro/programs/publichealth/oph_standards/docs/ophs_2021.pdf
Jumah, R., et al. (2023). Indigenous Lens Tool: Aligning health equity frameworks with Indigenous perspectives. Ontario Health. https://www.ontariohealth.ca
Ministry of Health and Long-Term Care. (2012). Health equity impact assessment (HEIA) tool. Ontario Ministry of Health. https://www.health.gov.on.ca/en/pro/programs/heia/
Ministry of Health and Long-Term Care. (2018). Health equity guideline. Ontario Ministry of Health and Long-Term Care. https://www.health.gov.on.ca
Ontario Health. (2025). Ontario Health Social Determinants of Health Framework & Resource Guide. Ontario Health. https://www.ontariohealth.ca